People are dying after procedures in NJ surgery centers and it's not always made public
 Lindy Washburn
Lindy Washburn
They are called “same-day surgery centers,’’ leading patients to expect a quick in-and-out for a routine procedure.
But the experience was anything but routine for Rekhaben Shah, 67, who reported to the Oak Tree Surgery Center in Edison for a colonoscopy. During the intestinal exam, her oxygen level plummeted and her pulse dropped. She died two days later.
Nor was it routine for Pedro Maldonado, 59, who went to the Ambulatory Care Center in Vineland for a seven-minute endoscopy to address stomach pain. He never woke up.
And not for Veronica Gates, 51, who scheduled surgery at the New Horizon Surgical Center in Paterson to relieve neck pain. Soon after she was put under, her family's lawsuit says, she suffered a heart attack and died.
The three cases constitute just a fraction of the thousands of procedures performed each day at New Jersey’s same-day surgical centers — freestanding operating facilities that increasingly take on complex cases without the safety net of a fully-equipped hospital.
Dozens of patients have died at the centers since the state began safety reporting in 2008, and more than a thousand patients have become comatose or suffered serious preventable injuries, state records show.

New Jersey has 298 such centers — more than New York, Connecticut or Pennsylvania. Until a 2010 state moratorium on creating new centers, it was easier to get permission to open a same-day surgery center in New Jersey than in most other states.
Doctors usually tell a patient where to have a procedure — whether inside a hospital or outside. And doctors like surgery centers because of their efficiency, ease of scheduling, and higher reimbursement from insurance companies and Medicare.
Most are owned by physicians, who receive a share of the “facility fee” as well as payment for procedures they perform. Higher out-of-network payments have been an added enticement, although many surgery centers now are included in insurance networks.
Patients and their insurers like surgery centers, too, because they promise lower costs, less risk of infection and greater convenience.
They count on the centers to offer the same protections and quality of care as hospitals.
But the two settings are different — in resources, regulations and oversight. And that can mean the difference between life and death.
Surgery at a same-day center can be like “walking on a tightrope with no safety net,” said Glenn Ellis, an attorney who filed a lawsuit on behalf of Pedro Maldonado, the Vineland patient who died. “The 1 percent of the time when it goes bad, it will go very bad because they have no safety net.”
Yet little information is available about the safety records of New Jersey’s free-standing surgery centers. The public has no way of knowing whether there have been problems, short of a special request to the state Health Department for inspection records or a trip to a county courthouse to look up malpractice lawsuits.
And even then, the information provided is scant and incomplete. The Record and NorthJersey.com looked up lawsuits and requested information via open public records requests. It found:
- More than 1,200 “events” — a neutral term that refers to death, falling into a coma during or after surgery, or serious preventable injuries that result in disability or other harm — were reported between September 2008, when the state began keeping count, and September 2017. No more specific breakdown of events is given.
- There were 52 people who died at New Jersey surgery centers between September 2008 and January 2017, according to an open-records request.
But those numbers likely understate the problems — perhaps by as much as half.

That’s because only half of New Jersey’s 300 surgical centers are required to report to the state’s Patient Safety Reporting System.
Due to a quirk in New Jersey law, surgery centers with only one operating room, like Oak Tree, where Rekhaben Shah had her colonoscopy, haven’t been licensed by the state Department of Health and haven’t been required to report their patient-safety data.
In all, 159 centers are not overseen by the Health Department, which inspects hospitals, nursing homes and other health facilities. Rather, they are overseen by the licensing board for doctors.
This two-tiered system is expected to end next January, when a law signed by former Gov. Chris Christie on his last day in office takes effect and a license from the Health Department will be required for all surgery centers, regardless of size.
Whether such oversight would have saved someone like Shah is unknown. But, like the thousands who use these centers each day, she had no easy way to check Oak Tree’s safety record before her procedure.
And because Oak Tree had only one operating room, what happened during her colonoscopy and subsequent death was not reported to New Jersey's Patient Safety Reporting System and is not part of the state's assessment of surgical-center safety.
It’s estimated a million procedures — from colonoscopies to cataract surgery, face-lifts to pain injections — are performed each year at ambulatory surgery centers in New Jersey, about 325,000 of them on Medicare patients. Soon, patients at these centers may be able to go home just hours after a total hip or knee replacement as Medicare expands the scope of what it will pay for outside a hospital.
Most people find that their surgeries or other procedures go well. More than half of the licensed same-day centers report no problems to the state. The industry trade group is proud of the quality of care they offer.
“You’re going to get highly specialized care in a safe environment,” said Andrew Weiss, past president of the New Jersey Association of Ambulatory Surgery Centers.
Patients should have fewer concerns about health-care-acquired infections, he said, because “you don't have issues that happen in an acute-care hospital with long-term patients who are very, very sick.” And patient satisfaction, measured by industry surveys, is high, he said.
Learn more:Patient Safety Reporting System annual and quarterly reports
New law:Bill approved in January 2018 changes rules
But unbeknownst to patients, there can be problems.
An investigation by The Record and NorthJersey.com that included a review of scores of inspection reports, licensing records, and legal documents filed in 20 lawsuits on behalf of victims, as well as dozens of interviews, has found:
- Surgery centers lack the resources of a hospital for dealing with emergencies. Some have been found by state inspectors to lack supplies or equipment needed to resuscitate patients when heart or breathing problems develop, or to help diagnose complications that may appear after surgery. Crucial time can be lost waiting for emergency medical workers or transporting a patient to a hospital.
- Some accept patients who ought to receive a hospital's more intensive monitoring and post-operative care, lawsuits claim.
- Some don't vet their doctors, who may be part-owners, and other professionals as rigorously as hospitals do, according to lawsuits and disciplinary records. They may not require specialty board certification or may be lax in enforcing the state regulation that requires physicians to maintain hospital privileges for procedures they perform in non-hospital settings.
- Unlicensed centers are inspected less frequently and the results may not be made public. Complaint inspections for unlicensed centers are not made public by the Board of Medical Examiners.
Of course, problems and mistakes occur at hospitals as well.
There were 38 surgery-related deaths reported at the state’s 72 hospitals in 2015, among some 670,000 inpatient and outpatient operations. Hospital patients are often sicker and frailer, and the surgery often much more complex, than at a surgical center.
That same year, 12 deaths and 161 serious preventable adverse events were reported by about 160 licensed surgery centers. Again, no data are available about deaths and “events” at the unlicensed centers.
“Any sentinel event, any occurrence, is taken very seriously,” said Weiss, the past industry association leader. “We're not trying to obscure or obfuscate data. We totally support transparency."
But there is a long way to go.
Linda Schwimmer, president of the New Jersey Health Care Quality Institute, said checking out a surgery center is like looking at a "black box." Her staff spent 13 months requesting inspection reports from state regulators about the facilities. The information available "is not usable for somebody making a decision," she said.
Reports to the state’s Patient Safety Reporting System by centers that do report are not available to the public, by law. That law is intended to encourage honest reporting of bad outcomes by shielding the identity of the victims and preventing the information from being used in lawsuits.
Medicare, the federal insurance program, has a “quality reporting” program that asks centers to report transfers to hospitals, so the public can make comparisons. But the data include only Medicare beneficiaries; transfers of other patients are not reflected.
By combing through court records of lawsuits filed by patients’ families it’s possible to get a partial picture of surgery centers’ safety gaps. But just a fraction of people harmed get a lawyer. And even court records don’t tell the full story, because most malpractice suits settle before trial, and their details remain confidential.
Buried within the courthouse files, however, are tragic stories. Here are three:

“Everything shattered” when her mother died, said Neha Shah, 42.
Rekhaben, known as Rekha, was the family matriarch, a guiding presence in the lives of her two children and their families. She cared for her husband and looked after two grandsons, 4 and 11, while their parents worked. She hadn’t wanted to get the colonoscopy exam, her daughter said, but accepted Neha’s reassurances it was routine.

“There was nothing wrong with her,” Neha said.
But her routine appointment at the Oak Tree Surgery Center in Edison led to disaster.
According to medical records, paramedics' reports and court depositions in the lawsuit her family has filed, this is what happened:
The colonoscopy began under anesthesia but was halted within a few minutes when Shah’s oxygen level dropped and kept sinking. Her heart slowed and blood pressure dropped.
A nurse started CPR. The colonoscopy doctor called 911.
An ambulance with a basic life-support crew was the first to arrive at the Oak Tree Surgery Center. When paramedics, who are trained in advanced life support, arrived seven minutes later, they found the ambulance crew in the foyer "reporting that staff in OR suite is refusing to let them enter the room," the paramedics report said.
The paramedics were allowed into the OR, where a paramedic described a “very chaotic scene" in her deposition for the family’s lawsuit.
They found "a staff member straddling [the patient] on table doing compressions and a female staff member who identifies herself as the anesthesiologist screaming for bicarb," their report said. Sodium bicarbonate was once used to treat cardiac arrest, but it has not been recommended by the American Heart Association for routine use since 2010.
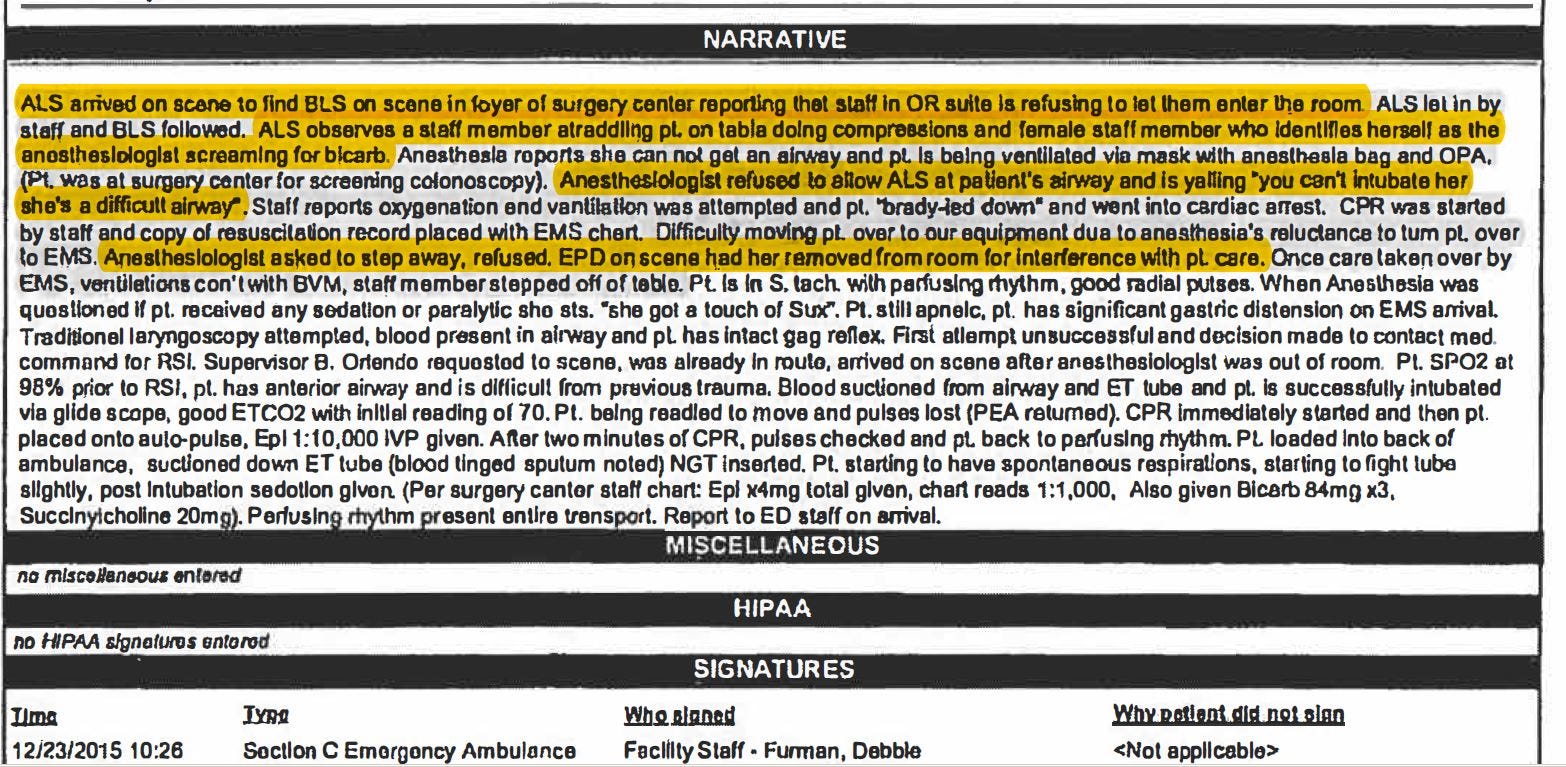
Above: The patient care report filed by paramedics from JFK Medical Center in Edison.
The anesthesiologist told the emergency responders she couldn't "get an airway" and was using the anesthesia mask and equipment to ventilate the patient, according to their report. "She wouldn't allow us near the patient," the paramedic said in her deposition. "She wouldn't listen to us when we asked her to move so we can get there."


The paramedic asked for help from the police officers who had responded to the call.
"EPD [Edison Police Department] on scene had her [the anesthesiologist] removed for interference with patient care," the paramedics’ report said.
The paramedics’ supervisor, who arrived at that moment, then used a device from his kit called a GlideScope to quickly intubate Shah. The device, which has a video screen to see into the airway, is common at hospitals, but the surgery center did not have one.
Shah’s pulse stopped again and the paramedics started CPR again, then rushed her to JFK Medical Center. Shah never regained consciousness and died two days later, on Christmas 2015.

Neha is haunted by memories of her dash to the hospital emergency department to meet the ambulance carrying her mother. When interviewed at the office of her lawyer Abbott Brown, she and her brother Kaushal said they hope to make the public aware of the risks of surgery centers. Their suit against the anesthesiologist, Dr. Yoori Yim, and Oak Tree Surgical Center is in court.
The Shah family’s expert said delays caused when Yim refused help "cost Mrs. Shah precious minutes” and that lack of oxygen caused her death. “Mrs. Shah died because of Dr. Yim’s conduct," the expert's report said.
A second expert said Shah “would be alive today” if the center “had maintained an inventory of appropriate and necessary airway management equipment.”
Yim and the surgery center have denied the lawsuit's claims, in legal filings.
The surgery center’s expert witness said that Shah’s condition — a rigid jaw and neck and a spasm blocking her airway — prevented Yim from opening Shah’s mouth and getting an airway tube in. There was no suggestion that Oak Tree had refused to purchase a GlideScope, his report said, and at any rate, they are not required at ambulatory surgery centers in New Jersey.
Oak Tree’s lawyer did not respond to requests for comment.

Yim's expert witness blamed the surgery center, and said that if the surgery center had had a GlideScope, “we would probably not be discussing this case at all." He described Yim’s actions as "timely and appropriate.” Her attorney, Thomas Heavey, declined to comment when contacted.
Yim settled an unrelated malpractice lawsuit for $700,000 in December 2016, according to state licensing records. Although legal records show that the state licensing board inquired about this case, she has not been disciplined.
Yim was asked during a deposition in August if she had blocked emergency medical personnel from working on her patient. "Not at all," Yim answered.
Asked why police had to oust her from the room, she said: "I wanted to stay in the room. … They don't want me to. I wanted to be a help to them."
She had not left voluntarily, she said, because "I was desperate. I wanted to help them to resuscitate the patient."
According to the deposition, Yim calls herself a "freelancer in anesthesiology." She works at several surgery centers as an independent contractor, she said, and hasn’t performed surgical anesthesia in a hospital since 2002.
On the day when Shah was stricken, legal filings show, Yim resumed her tasks at the center within an hour of Shah’s departure by ambulance. She handled patient anesthesia for eight more procedures.
Twenty months after Rekhaben Shah died, Yim was asked in a deposition when she had last worked at Oak Tree Surgery Center.
"A week ago," she said.
Veronica Gates, a 51-year-old hospital administrator, came to Paterson from Mechanicsville, Maryland, for neck surgery at a same-day center, choosing a surgeon whose record included multiple malpractice lawsuits and settlements.
She shouldn't have had the surgery outside of a hospital, her family's lawyer says.
After she died, state inspectors cited problems at the center.
Gates arrived at New Horizon Surgical Center, a licensed center located in the former Barnert Hospital, in February 2015. It’s unclear why she didn’t go to a surgeon closer to home for her neck pain. Her primary-care doctor in Maryland cleared her for the procedure.
Gates had aortic stenosis, a heart condition in which the valve from the heart to the main artery is narrowed and the heart must pump harder to send blood to the rest of the body, said attorney Paul Bekman of Baltimore.
She wasn't a good candidate for the operation, he said. But if she was going to have it, he said, "it should never have been done in a surgical center. It should have been done in a hospital, where there's intense monitoring and they could have intervened."
Soon after she was anesthetized, she developed an irregular heartbeat and went into cardiac arrest, he said.
According to her family's lawsuit, the surgical center "Failed to provide adequate resuscitation equipment."


Supplies of two drugs used for resuscitation — vasopressin and magnesium sulfate — were back-ordered and missing from the emergency carts in the operating room and post-anesthesia care unit, according to an inspection by New Jersey health officials five days after Gates died. The report was obtained by The Record through an open-records request. New Horizon subsequently corrected the problem, according to Health Department documents.
The deceased patient's husband went back to the surgery center the day after she died to complain about the care she’d received, according to the state's complaint inspection. But New Horizon had no record of his or other complaints, the report said. They didn’t keep a complaint book, a staffer told the inspector, because “they did not have any complaints.”
Gates' surgeon was Scott Katzman, an orthopedist with New Jersey Spine & Orthopedic who operates at several locations in Florida and New Jersey. Katzman has been sued by two other New Jersey residents for medical malpractice and several times in Florida, including once for a death after an operation he did at a surgery center. He has been disciplined by the Florida licensing board for failing to register two of his surgery centers appropriately for the high level of surgery he was doing in them, and subsequently reprimanded by California's medical board.
The Gates family's lawsuit, filed in state Superior Court in Essex County, named the Maryland primary-care doctor, B. Larry Jenkins Jr., who cleared Gates for surgery; the surgery center; Katzman; Jessica Isabel DeLamota, the anesthesiologist; and their medical practices.
Each has denied wrongdoing in court filings.
In a preliminary ruling, the court allowed Jenkins to be sued in New Jersey for malpractice, even though his medical license is from Maryland, said Barry D. Epstein, the Gates family’s local counsel. The case is still pending.
Lawyers for physicians Katzman, Jenkins and DeLamota did not respond to requests for comment, and New Horizon’s lawyer declined to comment.

Pedro Maldonado was losing weight because of terrible stomach pain, and his doctor wanted to examine his upper digestive tract with an endoscope. But Maldonado also had a pacemaker and a history of heart trouble.
A tragic combination of overconfidence and inattention led to his April 2015 death, a lawsuit filed in U.S. District Court by his widow, Carmen Carrasquillo, claims.

Among the problems alleged in the lawsuit:
- No cardiologist cleared Maldonado for the procedure.
- The anesthesiologist proceeded without speaking with Maldonado.
- When Maldonado didn’t wake up in the recovery room, emergency treatment was delayed.
The doctor who referred Maldonado to the Ambulatory Care Center in Vineland, Woo Kwang Song, was a part-owner of the facility, and allowed his financial interest to outweigh the best interests of his patient, the lawsuit alleges.
It is one of the first such cases to be filed under the federal anti-kickback law.
The lawsuit, filed by attorney Glenn Ellis, claims that the undisclosed financial incentives for the physician to refer patients to a center he owned in part — a center that failed to meet Medicare’s safety standards, the lawsuit says — mean its Medicare billings were fraudulent and should be repaid to the government.
Maldonado was 59 when he died, a doting grandfather and devout pastor in Vineland’s Puerto Rican community who left a government job on the island after a previous heart attack, his widow said.
When he went to the surgery center that morning, “he was desperate,” his widow said. “He has too much pain. He want[ed] to feel better.” He had visited Song, his gastroenterologist, twice, but nothing helped.
At his second visit, the doctor said, “Go to this center,” Carrasquillo said, and made the appointment for them.
The morning of the endoscopy, Maldonado ticked the boxes on the intake form for high blood pressure, heart trouble, previous heart attack, difficulty walking up stairs and other health problems, the lawsuit said. He added a note —“I have a fibrillator” — and said he wanted to speak with the anesthesiologist, according to court documents.

But Larry Feinerman, the anesthesiologist, did not speak to him before the procedure, the lawsuit said. Feinerman is not board-certified in anesthesiology, according to his deposition.
Before the procedure, the center’s nursing director later testified, the nursing director called the center’s medical director to say, “I did not feel he [Maldonado] was adequately prepared to be done in this facility.”
“I felt with his pacemaker and his previous cardiac history that he should have had a cardiac clearance,” said the nursing director, who no longer works there. But the medical director deferred to the anesthesiologist, according to the nursing director’s testimony.
The procedure took seven minutes.
In the recovery room, no one noticed Maldonado was unresponsive for 10 minutes, the lawsuit said. The staff had no “true crash cart” for such emergencies and did not begin CPR until 25 minutes had elapsed; Maldonado was not wheeled into the local hospital’s emergency room for another 27 minutes. the lawsuit said.
He never woke up.
Reached by phone, a center administrator declined to comment. In a legal filing, the center denied claims of wrongdoing. Attorneys for the physicians, Song and Feinerman, have also denied the lawsuit’s claims in legal filings. Song’s attorney has asked the court to dismiss a portion of the case.
A week later, Carrasquillo said, she decided to remove her husband from life support.
“I don’t want to talk a lot about it,” she said in an interview at her daughter’s home, weeping, “because it still hurts.”
All New Jersey surgery centers will soon play by the same rules, under a law signed by former Gov. Chris Christie on his last day in office.
The law will require more than 150 centers that currently operate without state licenses to get them.
They will be inspected more often – by officials from the state Health Department who have experience overseeing other types of health facilities – and the inspection results will be posted online.
That’s a first: about half of New Jersey’s 300 same-day surgery centers have been exempt from such oversight because they have only one operating room. They are considered extensions of the doctor’s office and registered with the physician licensing board, which does not make information about complaints public.
There is some evidence that the state’s unlicensed centers have had more safety problems.
Two-thirds of the unlicensed facilities – compared with one-third of the licensed facilities – surveyed in 2015 received "immediate jeopardy" citations, according to Medicare data.
That is the worst mark; it means inspectors believe the centers' failure to comply with safety regulations "has caused or is likely to cause serious injury, harm, impairment or death to a patient," according to Medicare regulations.
But the 2015 Medicare inspection reports, obtained through an open-public records request, provided just a small snapshot: only 36 of the 300 New Jersey surgical centers were included.
The data were consistent with the findings of a 2011 report by the New Jersey Health Care Quality Institute, however.
That year, the group found that 43 percent of the unlicensed surgical practices “were noncompliant with certain serious safety requirements,” compared with 15 percent of the licensed surgical centers. That was based on 91 surveys from 2009 and 2010.
“There is evidence that consumers may be at greater risk in unlicensed surgical practices than in licensed ASCs,” the institute concluded in 2011.

Few industry organizations ever ask for an increase in regulation, but the state trade group for ambulatory surgery centers was a strong advocate of fixing this patchwork system of oversight.
“We rigorously support transparency for all of the ambulatory surgery centers, registered or licensed,” said Andrew Weiss, past president of the Association of Ambulatory Surgery Centers of New Jersey. “This is a bill that had no stated opposition,” Mark Manigan, the group’s general counsel, said.
The centers have until next January to comply with the new law. The Health Department is hiring new staff.
"Shining a light on how they're doing will be more effective than anything else" in making ambulatory surgery centers pay attention to safety, said Linda Schwimmer, president of the New Jersey Health Care Quality Institute.
Health-care facilities that operate outside public scrutiny have little incentive to improve, experts say.
“A private assessment of the safety of a facility which is then kept from the public eye is no transparency at all,” an institute director testified earlier last year. “Consumers, employers, and purchasers have a right to the information necessary to decide where to go for care.”
Additional reporting by Christina Jewett of Kaiser Health News
♦ ♦ ♦ ♦ ♦
This story began last August with an invitation to participate in a USA Today Network investigation probing deaths at America's 5,300 freestanding ambulatory surgery centers. This national reporting project has been led by Kaiser Health News and the Indianapolis Star.
No national public repository of surgery center death cases exists.
Using an online database of lawsuits, reporters identified medical malpractice actions that involved both a death and an ambulatory surgery center. With that information in hand, The Record's reporter, Lindy Washburn, traveled to county courthouses in New Jersey to look up case files.
Washburn then reached out to plaintiffs' attorneys in those lawsuits to learn more about the cases. Most plaintiffs' attorneys did not return calls or declined to speak about their clients' cases. But a handful provided more information.
To get an idea of the scope of the problem, Washburn consulted the New Jersey Department of Health's Patient Safety Reporting System.
Although the state began requiring ambulatory surgery centers to report deaths and other adverse events in 2008, the information published on the department's web site was incomplete. An Open Public Records request for the data was made. But because only half of the state's same-day surgery centers — the licensed ones — participate in the reporting system, the numbers remain incomplete.
At the same time, information about the safety records of various centers in New Jersey was sought. National reporters obtained a massive database of inspection reports for centers that receive Medicare reimbursement.
Washburn extracted the New Jersey reports, and compared results in New Jersey for licensed and unlicensed centers. The inspection reports for the centers involved in each of the lawsuits also were obtained, using OPRA requests as needed.
Disciplinary records about each of the doctors involved in the highlighted cases were also obtained. Washburn called defense lawyers in the various cases and traveled with a photographer to interview the victims' families and their attorneys.
As all this was taking place, a bill made its way through the New Jersey Legislature to eliminate the state's two-tiered system of surgery-center oversight. Governor Christie signed that on his last day in office, giving our story its last chapter.
PROJECT CREDITS
Lindy Washburn has reported on health care in New Jersey for nearly 30 years. She was named New Jersey Journalist of the Year twice and has received numerous national and state awards for her reporting. In 2013, she received a year-long fellowship on health care performance from the Association of Health Care Journalists.
Daniel Sforza is the investigative editor at The Record and has overseen some of the paper's most ambitious reporting efforts, including the "Toxic Secrets" series about DuPont's legacy of contamination in a small North Jersey town; the coverage of the Bridgegate scandal, a story broken by The Record; the newspaper’s Pulitzer-finalist heroin coverage; and The Record's award-winning investigative coverage of NJ Transit.